July 10, 2007
Vertigo
SYMPTOM OVERVIEW
• Vertigo: a condition that is usually due to a disturbance or asymmetry in the vestibular system involving the semicircular canals or the central nervous system structures.
• Key anatomical components: semicircular canals (horizontal, posterior; superior); otolithic apparatus (utricle and saccule)
• Types of vertigo: Peripheral (80% of cases) and Central
• Peripheral vertigo: benign paroxysmal positional vertigo; Meniere's disease; Cogan's syndrome (see MMW link); otitis media; vestibular neuritis; acoustic neuroma; semicircular canal dehiscence syndrome; perilymphatic fistula; aminoglycoside toxicity; recurrent vestibulopathy; herpes zoster oticus; and labyrinthine concussion
• Central vertigo: multiple sclerosis; cerebellar infarction and hemorrhage; brainstem ischemia; migrainous vertigo; chiari malformation;
episodic ataxia type 2
SIGNS AND SYMPTOMS
• Nystagmus: a rhythmical oscillation of the eyeballs
o Horizontal: usually occurs in peripheral vertigo as illustrated by the horizontal security light beams surrounding the periphery of the diamond. However, horizontal nystagmus is occasionally noted in patients with poor pursuit due to large central lesions.
♣ Peripheral lesions: fast component away from affected side; visual fixation suppresses nystagmus (robber becomes focused on the diamond while standing in the periphery, thereby, stopping the nystagmus)
o Vertical (upbeat/downbeat): usually occurs in central vertigo as illustrated by the vertical security light beams shinning down on the central aspect of the diamond. However, central vertigo may present with various patterns of nystagmus.
• Central lesions: Nystagmus may reverse direction with convergence (convergence of vertical light beam on diamond)
• Caloric testing: Lack of a response to warm or cold water on one side suggests disease on that side, usually in peripheral lesions.
• Postural Instability
o Peripheral lesions: walking is usually preserved
o Central lesions: frequent falls occur while walking
• Auditory
o Peripheral lesions: deafness, tinnitus, or ear pain may occur
o Central lesions: rarely have auditory complaints
DIAGNOSIS
• Dix-Hallpike maneuver: useful for the confirmation of benign paroxysmal positional vertigo
• Audiometry: useful in the evaluation of peripheral lesions and in the confirmation of Meniere's disease.
• Imaging: MRI/MRA are useful in evaluation of central lesions. MRI/CT are useful in evaluating acute sustained vertigo in some circumstances.
The Tulio Phenomenon illustrated here consists of sound induced vertigo or nystagmus that can be caused by superior canal dehiscence; perilymphatic fistula; and Meniere's disease.
• A peripheral lesion in the inner ear may present with deafness and tinnitus.
TREATMENT
• Treatment of the underlying cause
• Symptomatic treatment duration of 48hrs or less with one of the following drug classes: anticholinergics; antihistamines; benzodiazepines; antiemetics observing potential drug –drug interactions
• Vestibular exercises/rehabilitation
Posted by mmw at 11:19 AM | Comments (0)
Bell's palsy
Posted by mmw at 10:53 AM | Comments (0)
January 29, 2007
Inclusion body myositis
Inclusion Body Myositits
Overview
• Most common inflammatory myopathy in the elderly
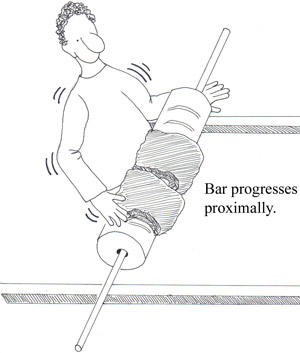
• Insidious onset of slowly progressive proximal and distal weakness (see fig 2)
• Usually after age 50 years old
• Men are more affected than women
Signs/Symptoms
• Early weakness and atrophy of the quadriceps (knee extensors); volar forearm muscles (wrist and finger flexors); and tibialis anterior (ankle dorsiflexors) muscles
• Asymmetrical muscle involvement
• Shoulder and hip girdle weakness
• Facial weakness ( 33% of patients)
• Dysphagia (50% of patients)
• Distal sensory peripheral neuropathy (30% of patients) (see fig 2)
• Quadricep muscle stretch reflexes are decreased if quadriceps atrophy is present
• Knee pain due genu recurvatum
Diagnosis
• Muscle biopsy
Treatment
• Supportive ( Usually refractory to immunosuppressive therapy intravenous gamma globulin therapy)
Prognosis
• Normal life expectancy
• Patients are usually incapacitated within 10 to 15 years of onset
Posted by mmw at 05:41 PM | Comments (0)
September 13, 2006
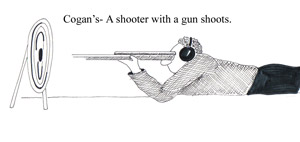
Cogan's Syndrome
DISEASE OVERVIEW
• combination of inflammatory eye disease and vestibuloauditory dysfunction
• rare autoimmune disorder affecting the inner ear
• described as Meniere's-like fluctuating hearing loss combined with impaired caloric response
• young adults commonly affected
• As many as 15% of CS patients have a large- to medium-vessel vasculitis
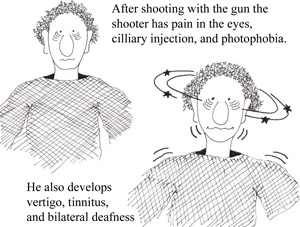
• As a helpful mnemonic device think of a man shooting a gun (rhymes with 'gan' in Cogan’s; see the side effects the shooter experiences in the figures below)
 SIGNS / SYMPTOMS
SIGNS / SYMPTOMS
• acute nonsyphilitic interstitial keratitis
• sensorineural hearing loss (see figure 3 below)
• Medium- and large-vessel arteritis (aortitis, aortic regurgitation, coronary artery inflammation, mesenteric vasculitis, and limb claudication)
• severe vertigo (see figure 3 below)
• nausea/ vomiting
• tinnitus
• diarrhea and/or bloody stools (10% patients with CS)
DIAGNOSIS
• clinical suspicion (make sure to consider more common diseases before committing to a diagnosis of CS)
TREATMENT
• systemic corticosteroids for inner ear disease (high doses)
• topical steroids for interstitial keratitis
• cytotoxic agents for cases refractory to corticosteroids
Posted by mmw at 09:36 PM | Comments (0)
September 11, 2006
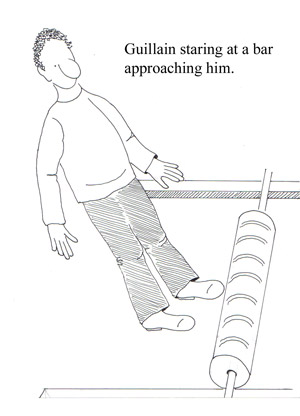
Guillain Barre Syndrome
DISEASE OVERVIEW
• Group of autoimmune syndromes consisting of demyelinating and acute axonal degenerating forms of the disease
• Rapidly evolving polyradiculoneuropathy preceded by a triggering event, most often an infection
• Incidence: 1 to 3 per 100,000 persons annually
• Campylobacteriosis is the most common precipitant in GBS
• Influenza vaccine is associated with a risk of 1-2 cases GBS per 1 Million
SIGNS/SYMPTOMS
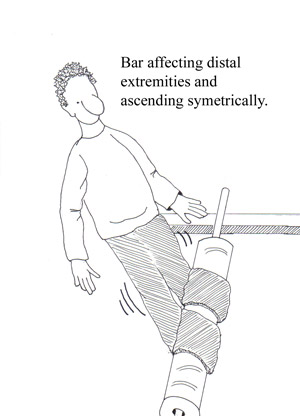
• Progressive, symmetric neurologic symptoms
• Weakness (proximal muscles; legs more often than arms) see figures below
• Tingling dysesthesias (extremities)
• Paresthesias (spread proximally) see figures below
• Disappearance of deep tendon reflexes (within the first few days of symptom onset)
• Cranial nerve involvement may affect airway maintenance, facial muscles, eye movements, and swallowing
• Pain (shoulder girdle, back, and posterior thighs) See fig 3 below
DIAGNOSIS
• a definitive diagnosis is usually not possible until the fifth day after the onset of symptoms
• Clinical features: progressive weakness in both arms and legs; areflexia
• CSF findings: elevated protein (greater than 0.55 g / dL ) without pleocytosis
• Electrodiagnostic findings: an absent H reflex, low amplitude or absent sensory nerve action potentials, an abnormal F wave, and other less frequent abnormalities
TREATMENT
• All patients who have GBS should be admitted to a hospital for close observation for respiratory compromise, cranial nerve dysfunction, and autonomic instability
• Monitor lung function
• Physical therapy
• Pain control with narcotics along with carbamazepine or gabapentin
• High-dose intravenous immunoglobulin (IVIg; 400 mg per kg daily for five days)
• Plasmapheresis (five exchanges over five to eight days) OR IVIG
Posted by mmw at 09:29 PM | Comments (0)
July 30, 2006
Syringomyelia
DISEASE OVERVIEW
Syringomyelia is a clinical syndrome created by a cavity which forms within the spinal cord resulting in the destruction of segmental neurons and long ascending and descending tracts passing through the involved spinal segments. The cavity which forms within the spinal column is called a syrinx (Gr: pipe). A syrinx is cavity is like a pipe or syringe within the gray matter of the spinal column. The two types of syringomyelia are hydromyelia (communicating) and posttraumatic syringomyelia (noncommunicating). The course is usually chronic and progressive.
TYPES
• Posttraumatic: occurs in approximately 3% of patients with spinal cord injury
SIGNS and SYMPTOMS
• Symptoms usually begin in the hands and arms (note swimmer diving in hands first)* because of the involvement of the central lower cervical spinal cord.
• Hyporeflexia in upper extremities: due to destruction of the dorsal horn fibers from muscle stretch receptors
• Loss of pain and temperature perception (hands and arms): destruction of dorsal horn fibers from pain receptors
• Position, vibration, and touch sensation are usually preserved
• Upper extremity muscle weakness and atrophy: destruction of motor neurons and the anterior gray horns
• Lower extremity spastic weakness: occurs as long ascending and descending pathways are compressed by the expanding syrinx
• As the syrinx increases in diameter, long ascending and descending pathways passing through the involved cord segment are compressed or invaded by the cavity and cause spastic weakness of the legs. Tracts to and from the sacral bladder centers are spared, or involved late in the disease, so that bladder symptoms occur late or not at all.
• Central neuropathic pain
• Headache and neck pain
• Autonomic symptoms (interruption of intermediaolateral column): Horner’s syndrome and trophic changes of the skin

DIAGNOSIS
• Spinal MRI with contrast : reveals a central spinal cord cavity
• Electrophysiology: denervation in affected segments
TREATMENT
• Neurosurgical: Budd Chiari malformation – foramen magnum decompression
Posttraumatic - shunt
Posted by mmw at 06:28 PM | Comments (0)