« August 2006 | Main | October 2006 »
September 25, 2006
Antinuclear antibody patterns
OVERVIEW
• Antinuclear antibodies (ANA): autoantibodies directed against histones, double-stranded and single-stranded DNA, ribonucleoprotein (RNP) complexes, and other nuclear components.
• Indirect immunofluorescence assays detect antibodies that bind to various nuclear antigens, and are used to report the titer of the ANA and the pattern of nuclear staining of the ANA.
• Titers 1:40 are considered positive.
• Titers 1:320 are more likely to represent true-positive results.
• There are various staining patterns
STAINING PATTERNS
• Diffuse / homogeneous: antibodies to histone (see bubbles in glass “think of histone subunits floating in the glass”)
• Rim: antibodies to nuclear envelope proteins and to double-stranded (ds) DNA (see salt on the rim of the glass)
• Speckled: antibodies to Sm, RNP, Ro/SS-A, La/SS-B, and other antigens (see speckled particle in the glass)
• Nucleolar: associated with diffuse scleroderma
• Centromeric: highly specific for the CREST syndrome
ANTIBODIES TO HISTONE
• Drug induced lupus: Anti-histone antibodies are sensitive but nonspecific for drug-induced lupus
• Anti-histone antibody testing may be useful in patients with a positive ANA test and a history of exposure to medications associated with drug-induced lupus (i.e. procainamide, isoniazid, hydralazine).
ANTIBODIES TO DOUBLE-STRANDED DNA (dsDNA)
• Antibodies to dsDNA recognize its base pairs, its ribose-phosphate backbone, and the structure of its double helix
• Systemic Lupus Erythematous (SLE): High titers of anti-double-stranded DNA (anti-dsDNA) antibodies are highly specific SLE (present in 60% of patients with SLE)
• Antibodies to dsDNA should be measured when there is clinical suspicion of SLE and the ANA is positive
• Specificity of anti-dsDNA antibodies for SLE is 97% overall and approaches 100% when the antibody titer is high
ANTI-SMALL NUCLEAR RIBONUCLEOPROTEINS
• Anti-Sm (anti-Smith) antibodies: specific for SLE (20 - 30 % of SLE patients)
• Anti-U1 snRNP : SLE (30 - 40 %); myositis; esophageal hypomotility; sclerodactyly; Raynaud's phenomenon; arthralgias; arthritis; and mixed connective tissue disease (MCTD)
• Testing for anti-U1 snRNP should be limited to patients with a positive ANA test who are suspected of having SLE or MCTD
ANTI- Ro/SS-A and ANTI -La/SS-B
• Antibodies to La almost always occur in association with anti-Ro antibodies
• Anti-Ro/SS: Primary Sjögren's syndrome (SS); positive in 40-50%
• Anti-La : SLE (10 to 15 percent of patients); late-onset SLE; secondary Sjögren's syndrome; congenital complete heart block (90%);and neonatal lupus syndrome (70%)
• RNA-protein conjugates
• Ro and La refer to the antigen as localized to the cytoplasm
• SS-A and SS-B are nuclear antigens
ANTI-CENTROMERE
• Antibody to the kinetechore of chromosomes
• Scleroderma (22 – 36%)
• Raynaud's phenomenon
• CREST syndrome (15%)
• Primary biliary cirrhosis
Posted by mmw at 05:58 PM | Comments (0)
September 17, 2006
Quinolones
MECHANISM OF ACTION
• Bactericidal
• Inhibit bacterial DNA gyrase, topoisomerase IV, and two type II DNA topoisomerase enzymes
• For many gram-positive bacteria (such as S. aureus), topoisomerase IV is the primary activity inhibited by the quinolone (see gyrating dancers below)
• For many gram-negative bacteria (such as E. coli), DNA gyrase is the primary activity inhibited by the quinolone (see "queen" below stopping the gyrating dancers)
ABSORPTION/EXCRETION
• Quinolones are well absorbed after oral administration and are distributed widely in body tissues
• Bioavailability: for the fluoroquinolones it is greater than 50% for all agents and greater than 95% for several
• Volume of distribution: (high) The concentrations of quinolones in urine, kidney, lung and prostate tissue, stool, bile, and macrophages and neutrophils are higher than serum levels. Quinolone concentrations in cerebrospinal fluid, bone, and prostatic fluid are lower than in serum.
• Excretion: Most quinolones are cleared predominantly by the kidney, and dosages must be adjusted for renal failure. However, pefloxacin and moxifloxacin are metabolized predominantly by the liver and should not be used in patients with hepatic failure.

ANTIMICROBIAL SPECTRUM
• bactericidal against: E. coli and various species of Salmonella, Shigella, Enterobacter, Campylobacter, and Neisseria
• Third generation fluoroquinolones : levofloxacin, moxifloxacin, and gatifloxacin. They possess antibacterial activity against Chlamydia, Legionella, and Mycoplasma species, streptococcal, staphylococcal pathogens, and variable activity against E. faecalis
THERAPEUTIC USES
• Prostatitis: Norfloxacin, ciprofloxacin, and ofloxacin
• Sexually Transmitted Diseases: activity in vitro against N. gonorrhoeae, C. trachomatis, and H. ducreyi
• Gastrointestinal infections: traveler's diarrhea (frequently caused by enterotoxigenic E. coli)
• Respiratory infections: Community acquired/atypical pneumonia ; gatifloxacin and moxifloxacin have activity against S. pneumoniae. Quinolones also have in vitro activity against the rest of the commonly recognized respiratory pathogens, including H. influenzae, Moraxella catarrhalis, S. aureus, M. pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila
• Other infections: Ciprofloxacin received wide usage for the prophylaxis of anthrax and has been shown to be effective for the treatment of tularemia
• Urinary Tract Infection
ADVERSE REACTIONS
• Gastrointestinal: mild nausea, vomiting, and/or abdominal discomfort (3% to 17% of patients).
• CNS: mild headache and dizziness (0.9% to 11% of patients)
• Dermatology: Rashes; photosensitivity reactions
• Achilles tendon rupture or tendonitis (rare)
• Cardiac: QTc interval (QT interval corrected for heart rate) prolongation has been observed with sparfloxacin and to a lesser extent with gatifloxacin and moxifloxacin
• Endocrine: hypoglycemia has been reported in diabetic patients receiving insulin or glyburide plus fluoroquinolones
Posted by mmw at 10:09 PM | Comments (0)
September 13, 2006
Cogan's Syndrome
DISEASE OVERVIEW
• combination of inflammatory eye disease and vestibuloauditory dysfunction
• rare autoimmune disorder affecting the inner ear
• described as Meniere's-like fluctuating hearing loss combined with impaired caloric response
• young adults commonly affected
• As many as 15% of CS patients have a large- to medium-vessel vasculitis
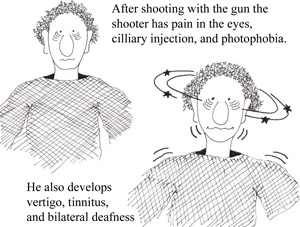
• As a helpful mnemonic device think of a man shooting a gun (rhymes with 'gan' in Cogan’s; see the side effects the shooter experiences in the figures below)
 SIGNS / SYMPTOMS
SIGNS / SYMPTOMS
• acute nonsyphilitic interstitial keratitis
• sensorineural hearing loss (see figure 3 below)
• Medium- and large-vessel arteritis (aortitis, aortic regurgitation, coronary artery inflammation, mesenteric vasculitis, and limb claudication)
• severe vertigo (see figure 3 below)
• nausea/ vomiting
• tinnitus
• diarrhea and/or bloody stools (10% patients with CS)
DIAGNOSIS
• clinical suspicion (make sure to consider more common diseases before committing to a diagnosis of CS)
TREATMENT
• systemic corticosteroids for inner ear disease (high doses)
• topical steroids for interstitial keratitis
• cytotoxic agents for cases refractory to corticosteroids
Posted by mmw at 09:36 PM | Comments (0)
September 11, 2006
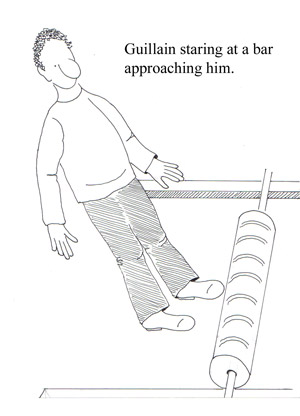
Guillain Barre Syndrome
DISEASE OVERVIEW
• Group of autoimmune syndromes consisting of demyelinating and acute axonal degenerating forms of the disease
• Rapidly evolving polyradiculoneuropathy preceded by a triggering event, most often an infection
• Incidence: 1 to 3 per 100,000 persons annually
• Campylobacteriosis is the most common precipitant in GBS
• Influenza vaccine is associated with a risk of 1-2 cases GBS per 1 Million
SIGNS/SYMPTOMS
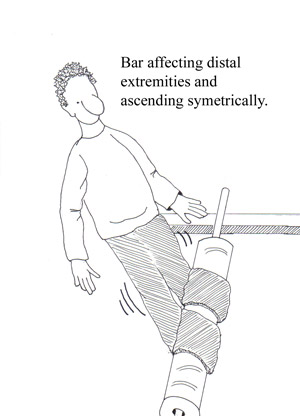
• Progressive, symmetric neurologic symptoms
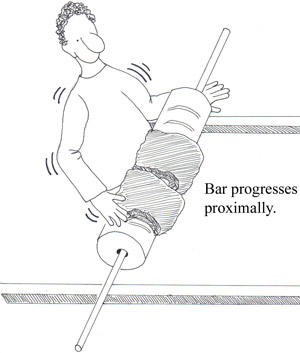
• Weakness (proximal muscles; legs more often than arms) see figures below
• Tingling dysesthesias (extremities)
• Paresthesias (spread proximally) see figures below
• Disappearance of deep tendon reflexes (within the first few days of symptom onset)
• Cranial nerve involvement may affect airway maintenance, facial muscles, eye movements, and swallowing
• Pain (shoulder girdle, back, and posterior thighs) See fig 3 below
DIAGNOSIS
• a definitive diagnosis is usually not possible until the fifth day after the onset of symptoms
• Clinical features: progressive weakness in both arms and legs; areflexia
• CSF findings: elevated protein (greater than 0.55 g / dL ) without pleocytosis
• Electrodiagnostic findings: an absent H reflex, low amplitude or absent sensory nerve action potentials, an abnormal F wave, and other less frequent abnormalities
TREATMENT
• All patients who have GBS should be admitted to a hospital for close observation for respiratory compromise, cranial nerve dysfunction, and autonomic instability
• Monitor lung function
• Physical therapy
• Pain control with narcotics along with carbamazepine or gabapentin
• High-dose intravenous immunoglobulin (IVIg; 400 mg per kg daily for five days)
• Plasmapheresis (five exchanges over five to eight days) OR IVIG
Posted by mmw at 09:29 PM | Comments (0)